Discharge Instruction Sheet Turp Patient 2004-2026 free printable template
Show details
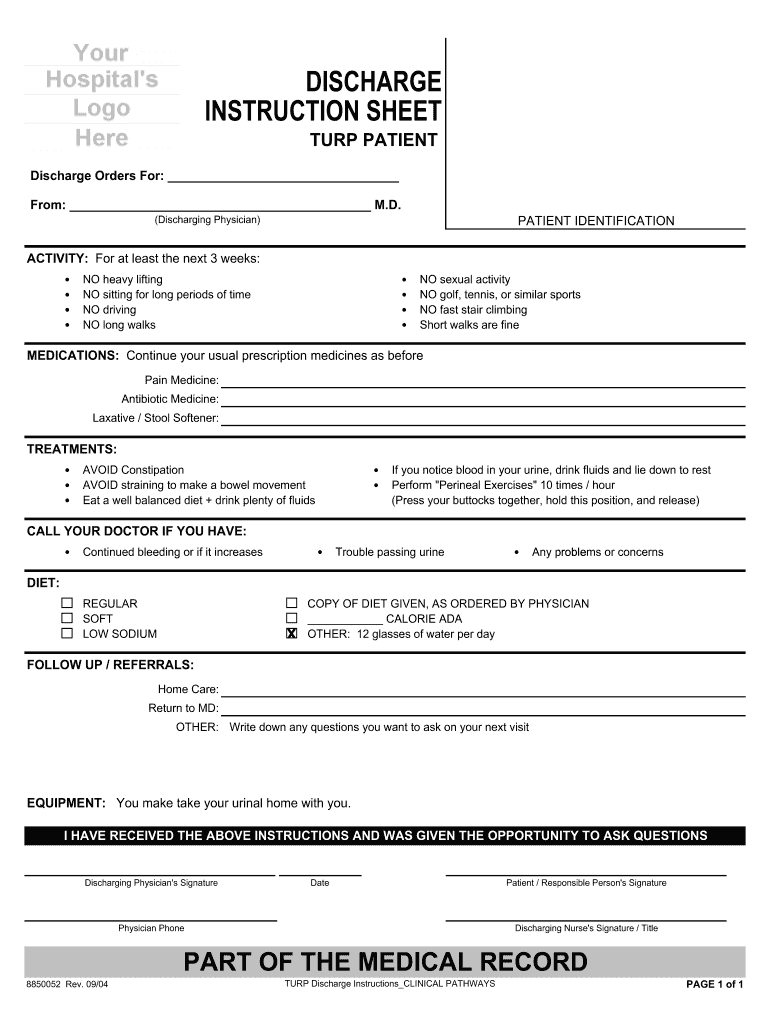
DISCHARGE INSTRUCTION SHEET TURP PATIENT Discharge Orders For From M. D. PATIENT IDENTIFICATION Discharging Physician ACTIVITY For at least the next 3 weeks NO heavy lifting NO sitting for long periods of time NO driving NO long walks NO sexual activity NO golf tennis or similar sports NO fast stair climbing Short walks are fine MEDICATIONS Continue your usual prescription medicines as before Pain Medicine Antibiotic Medicine Laxative / Stool Softener TREATMENTS AVOID Constipation AVOID...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign hospital discharge papers pdf form

Edit your hospital discharge papers pdf download form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your discharge papers hospital form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit real hospital discharge papers online
To use our professional PDF editor, follow these steps:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit discharge paperwork from hospital form. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
Dealing with documents is simple using pdfFiller. Try it now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out discharge paper form

How to fill out Discharge Instruction Sheet Turp Patient
01
Start by filling out the patient's name and medical record number at the top of the sheet.
02
Record the date of discharge and any relevant follow-up appointment information.
03
Provide clear instructions on medication, including dosage and frequency.
04
Outline any changes in diet or fluid intake post-surgery.
05
Include instructions for wound care and any signs of infection to watch for.
06
Specify activity restrictions or guidelines for physical activity.
07
Detail when the patient should seek emergency care or contact a healthcare provider.
08
Ensure the patient has a copy for their records and understands the instructions.
Who needs Discharge Instruction Sheet Turp Patient?
01
Patients who have undergone Transurethral Resection of the Prostate (TURP) surgery.
02
Caregivers or family members involved in the patient's post-operative care.
03
Healthcare providers involved in the patient's follow-up care.
Fill
discharge papers from hospital
: Try Risk Free






People Also Ask about discharge certificate from hospital pdf
How do I write a discharge paper?
When creating a discharge plan, be sure to include the following: Client education regarding the patient, their problems and needs, and description of what to do, how to do it, and what not to do. History of the hospitalization and an explanation of test data and in-hospital procedures.
What should be included in a discharge report?
6 Components of a Hospital Discharge Summary Reason for hospitalization: description of the patient's primary presenting condition; and/or. Significant findings: Procedures and treatment provided: Patient's discharge condition: Patient and family instructions (as appropriate): Attending physician's signature:
How do I get DD-214 discharge papers?
If you need assistance obtaining your military records, then contact any County Veteran Service Officer (CVSO). To obtain your DD-214 on your own, submit your request via the National Archives and Records Administration webpage or call 314-801-0800.
What makes a good discharge summary?
Thus, the Discharge Summary has pretty clear mandatory elements: what was the patient's history, why were they hospitalized, what were the significant events during their stay including procedures and treatments, in what condition did the patient leave the hospital, and what sort of follow-ups are required after
What should be included in discharge instructions?
A written transition plan or discharge summary is completed and includes diagnosis, active issues, medications, services needed, warning signs, and emergency contact information. The plan is written in the patient's language.
Can I get my discharge papers?
Yes. You can request your military records in any of these ways: Mail or fax a Request Pertaining to Military Records (Standard Form SF 180) to the National Personnel Records Center (NPRC).
What is a discharge letter from hospital?
A hospital discharge letter is a brief medical summary of your hospital admission and the treatment you received whilst in hospital.It is usually written by one of the ward doctors.
What is discharge paperwork?
Hospital discharge summaries serve as the primary documents communicating a patient's care plan to the post-hospital care team. 1, 2. Often, the discharge summary is the only form of communication that accompanies the patient to the next setting of care.
Who completes a discharge summary?
The MD/DO or other qualified practitioner with admitting privileges in ance with state law and hospital policy, who admitted the patient is responsible for the patient during the patient's stay in the hospital. This responsibility would include developing and entering the discharge summary.
What is a discharge summary?
A discharge summary is a clinical report prepared by a health professional at the conclusion of a hospital stay or series of treatments. It is often the primary mode of communication between the hospital care team and aftercare providers.
Why is a discharge letter important?
Sharing accurate, relevant information about the care received in hospital with primary care in the form of a discharge summary is essential to patient safety. This process inherently involves inter-professional communication which has been previously suggested as an area that requires improvement [5, 6].
Is a discharge summary a medical record?
The Discharge Summary is the most important document in the medical record. The Discharge Summary is the first document hospital coders review when they start coding any given hospitalization. The Discharge Summary is considered the final diagnostic statement for the entire hospitalization.
What should be on a discharge letter?
Most discharge letters include a section that summarises the key information of the patient's hospital stay in patient-friendly language, including investigation results, diagnoses, management and follow up. This is often given to the patient at discharge or posted out to the patient's home.
What is included in a hospital discharge summary?
The discharge report must give a summary of everything the patient went through during the hospital admission period – physical findings, laboratory results, radiographic studies and so on. An AHRQ study points out that the Joint Commission mandates six components to be present in all U.S. hospital discharge summaries.
What is hospital discharge summary?
A discharge summary is a handover document that explains to any other healthcare professional why the patient was admitted, what has happened to them in hospital, and all the information that they need to pick up the care of that patient quickly and effectively.
What is included in a discharge report?
The discharge report must give a summary of everything the patient went through during the hospital admission period – physical findings, laboratory results, radiographic studies and so on. An AHRQ study points out that the Joint Commission mandates six components to be present in all U.S. hospital discharge summaries.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit how to get discharge papers from hospital from Google Drive?
By integrating pdfFiller with Google Docs, you can streamline your document workflows and produce fillable forms that can be stored directly in Google Drive. Using the connection, you will be able to create, change, and eSign documents, including emergency room discharge papers, all without having to leave Google Drive. Add pdfFiller's features to Google Drive and you'll be able to handle your documents more effectively from any device with an internet connection.
How do I edit hospital discharge paperwork online?
The editing procedure is simple with pdfFiller. Open your discharge paperwork in the editor. You may also add photos, draw arrows and lines, insert sticky notes and text boxes, and more.
How do I edit hospital discharge form on an iOS device?
Create, edit, and share medical dischage letter pdf from your iOS smartphone with the pdfFiller mobile app. Installing it from the Apple Store takes only a few seconds. You may take advantage of a free trial and select a subscription that meets your needs.
What is Discharge Instruction Sheet Turp Patient?
The Discharge Instruction Sheet for a TURP patient is a document that provides essential information and guidelines for patients who have undergone Transurethral Resection of the Prostate (TURP) surgery. It includes instructions on post-operative care, medication management, and signs of complications.
Who is required to file Discharge Instruction Sheet Turp Patient?
Typically, the healthcare provider or nurse responsible for the patient's care during their hospital stay is required to file the Discharge Instruction Sheet for a TURP patient. This ensures that the patient receives the necessary post-operative instructions before leaving the facility.
How to fill out Discharge Instruction Sheet Turp Patient?
To fill out the Discharge Instruction Sheet for a TURP patient, healthcare providers should include the patient's name, date of the procedure, medications prescribed, dosage instructions, follow-up appointment details, and specific post-operative care instructions. Additionally, information regarding potential complications and when to seek medical help should be provided.
What is the purpose of Discharge Instruction Sheet Turp Patient?
The purpose of the Discharge Instruction Sheet for a TURP patient is to ensure that patients receive clear, concise, and accurate information about their post-operative care. This helps in promoting recovery, preventing complications, and providing a written reference for the patient to follow at home.
What information must be reported on Discharge Instruction Sheet Turp Patient?
The information that must be reported on the Discharge Instruction Sheet for a TURP patient includes the patient's demographic details, procedure date, prescribed medications, instructions for care at home, potential side effects, warning signs of complications, and the follow-up care plan.
Fill out your Discharge Instruction Sheet Turp Patient online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Printable Fillable Real Hospital Discharge Papers is not the form you're looking for?Search for another form here.
Keywords relevant to hospital discharge certificate pdf download
Related to the discharge instruction sheet should communication regarding post operative care
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.